Why Fructose is the Liver's Kryptonite: The Metabolic Disadvantage
- S A

- Nov 11, 2024
- 7 min read
Updated: Feb 25, 2025
Fructose, often found in sugary foods and drinks, has been called the “liver’s kryptonite” due to its unique, and often detrimental, metabolic effects. Unlike glucose, which fuels the entire body, fructose is primarily processed by the liver. This creates a distinct metabolic load, leading to an increased risk of fatty liver, insulin resistance, and obesity when consumed in excess (more on this further down). This blog (1) explores the journey of fructose in the body, how fructose metabolism differs from glucose metabolism, highlighting why fructose is particularly adept at promoting fat storage and how it disrupts metabolic health, contributing to obesity and metabolic disorders.
Fructose vs. Glucose: A Tale of Two Sugars
Feature | Glucose | Fructose |
Pathway | Glycolysis (throughout the body) | Fructolysis (Primarily processed in the liver) |
Insulin Signal | Stimulates insulin release | Minimal impact on insulin release |
Fat Production | Lower | High (through de novo lipogenesis) |
Source | Carbohydrates, some fruits | Fruits, high fructose corn syrup (processed foods) |
Glucose: The Body's Preferred Fuel
Glucose, a simple sugar found in carbohydrates, is the body's primary source of energy. Here's how it's processed:
The Glycolysis Pathway: Glucose enters a metabolic pathway called glycolysis, occurring primarily in the cytoplasm of cells throughout the body. During glycolysis, glucose is broken down into usable energy (ATP) and pyruvate, a molecule that can be further processed for energy or converted into other substances the body needs.
Regulation by Insulin: The hormone insulin plays a key role in glucose metabolism. When blood sugar levels rise after eating, the pancreas releases insulin. Insulin acts like a key, unlocking cells throughout the body to allow glucose entry. This ensures that glucose is readily available for energy production.
Fructose: A Different Metabolic Path
Fructose, another simple sugar found in fruits and high fructose corn syrup, takes a different metabolic route:
Fructose's Journey: Fructose bypasses glycolysis (it undergoes fructolysis) and heads straight for the liver. Here, it undergoes a series of enzymatic reactions, ultimately being converted into fat or glycogen (for short-term energy storage).
The Downside of Fructose's Shortcut
While fructose's direct journey to the liver seems efficient, it presents several disadvantages that contribute to fat storage and fatty liver disease:
No Insulin Signal: Unlike glucose, fructose doesn't stimulate the release of insulin to the same extent. This disrupts the body's ability to regulate blood sugar levels effectively.
Fat Production on Autopilot: The liver readily converts excess fructose into fat through a process called de novo lipogenesis. This newly created fat is then stored, often accumulating in the liver itself, contributing to fatty liver disease.
Fructose Overload: Our modern diet often contains excessive amounts of fructose, especially from high fructose corn syrup. This influx overwhelms the liver's ability to process it efficiently, further promoting fat production.
Fructose From Friend to Foe: Why Whole Fruits are Different
We've explored how fructose metabolism differs from glucose and its potential to promote fat storage and fatty liver disease. But hold on, aren't fruits also a source of fructose?
Fruits naturally contain fructose, but unlike processed sources, they come packaged with a key player: fiber. Here's why whole fruits are a different story:
Fiber's Slowdown Effect: Fiber slows down the absorption of sugar, including fructose, into the bloodstream. This gradual release prevents blood sugar spikes and gives the liver time to process the fructose more efficiently.
The Gut's Filtering System: The fiber in fruits also plays a role in the gut. It feeds the beneficial gut bacteria, which can further impact how fructose is metabolised.
A Package Deal: Fruits come packed with essential nutrients, including vitamins, minerals, and antioxidants, which can offset some of the downsides of fructose. Among these, quercetin—a flavonoid found in apples and other fruits—can help counteract the effects of uric acid, a byproduct of fructose metabolism that contributes to fat storage and metabolic stress. Quercetin's mechanism resembles that of allopurinol, a pharmaceutical drug used to lower uric acid levels in gout patients. Both quercetin and allopurinol inhibit xanthine oxidase, an enzyme that produces uric acid, thereby reducing oxidative stress and potentially minimising fructose’s negative metabolic impact.
The Gut: A Checkpoint for Fructose
The gut microbiome, the community of bacteria residing in our intestines, plays a role in fructose metabolism. Here's how:
Fructose and the Gut Bacteria: Some gut bacteria can actually ferment fructose, utilising it for energy production. This can help reduce the amount of fructose reaching the liver for processing.
Fiber's Fermentation Feast: The fiber in fruits provides sustenance for these beneficial gut bacteria, promoting a healthy gut microbiome and potentially aiding in fructose management.
The Downside of Liquid Fructose: Bypassing the Checks and Balances
Processed foods and sugary drinks often contain high fructose corn syrup, a concentrated source of fructose. Here's why this can be problematic:
The Fiber Factor: Unlike whole fruits, processed foods and sugary drinks lack fiber. This rapid influx of pure fructose overwhelms the gut's ability to regulate its absorption and sends it directly to the liver for processing.
Liver Overload: The liver can become overloaded with the surge of fructose from these processed sources, leading to de novo lipogenesis (fat production) and potentially contributing to fatty liver disease.
Increased Overall Calorie Intake: Sugary drinks and processed foods are often high in calories, leading to weight gain and potentially fatty liver disease. Insulin resistance can also contribute to weight gain by making it harder for the body to burn fat for energy.
Fat Production on High Gear: Fructose's metabolic pathway bypasses the steps that normally signal satiety (feeling full). This can lead to overeating and increased calorie intake. Furthermore, the liver converts excess fructose into fat through a process called de novo lipogenesis. This newly created fat is then stored, often accumulating in the liver itself, contributing to fatty liver disease.
Hidden Sugars: Many seemingly healthy foods can harbor hidden sugars. Consuming these can contribute to excess sugar intake and its associated health risks.
The Link to Fatty Liver Disease
Fatty liver disease develops when excess fat accumulates in the liver. As mentioned earlier, fructose consumption can directly contribute to this condition through de novo lipogenesis. Furthermore, insulin resistance caused by fructose can exacerbate fatty liver disease:
Impaired Fat Breakdown: Insulin normally signals the body to break down stored fat for energy. With insulin resistance, this process becomes less efficient, leading to further fat accumulation in the liver.
Increased Inflammation: Insulin resistance can trigger chronic low-grade inflammation throughout the body, including in the liver. This inflammation can damage liver cells and worsen fatty liver disease.
The Fructose Floodgate:
Our modern diet often contains excessive amounts of fructose, especially from high fructose corn syrup found in sugary drinks and processed foods. This influx creates a situation where the liver becomes overloaded:
Beyond Processing Capacity: The liver can only process a limited amount of fructose efficiently. When the intake exceeds this capacity, the liver struggles to keep up. The overloaded liver resorts to a process called de novo lipogenesis to deal with the excess fructose.
Fructose to Fat Conversion: The liver converts the extra fructose into fat. This newly created fat is then stored, often accumulating within the liver cells themselves. Over time, this fat buildup leads to a condition called non-alcoholic fatty liver disease (NAFLD). initially a silent threat, can trigger a cascade of negative effects when left unchecked
Inflammation on the Rise: Excess fat accumulation in the liver can trigger chronic low-grade inflammation, further damaging liver cells and worsening NAFLD.
Insulin Resistance: A fatty liver can impair insulin signalling, making it harder for the body to regulate blood sugar levels. This can lead to type 2 diabetes.
Metabolic Disruption: NAFLD can disrupt overall metabolism, affecting how the body processes nutrients and stores fat. This can contribute to weight gain and other health problems.
Scarring and Cirrhosis: In severe cases, chronic inflammation and damage can lead to scarring (cirrhosis) of the liver tissue, significantly impairing liver function. Liver failure can be a potential consequence of advanced cirrhosis.
Increased Risk of Cancer: Fatty liver disease and chronic inflammation are associated with an increased risk of developing liver cancer.
The Vicious Cycle: A vicious cycle can develop. Fructose overload leads to fatty liver, which, in turn, can worsen insulin resistance and further promote fat storage. This cycle can significantly increase your risk of developing serious health problems.

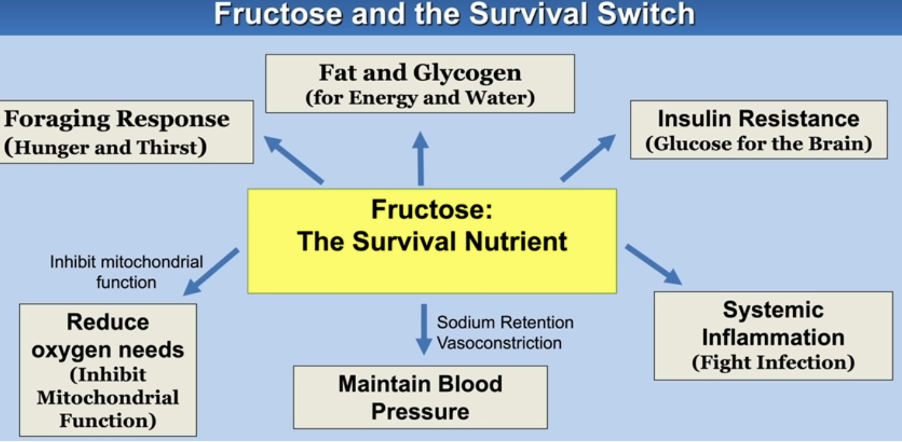
Image Credit: 10.1007/s00204-016-1892-7
Evolution Didn't Prepare Us for a Fructose Flood
Our bodies evolved to handle small amounts of fructose naturally found in fruits. However, our modern diet is overloaded with processed foods and sugary drinks, creating a fructose overload that disrupts our metabolism.
Breaking the Cycle: Protecting Your Liver
By limiting fructose intake, particularly from processed sources, can help us make informed dietary choices and can help prevent or manage fatty liver disease and safeguard your overall health:
Read Food Labels: Pay close attention to added sugar content on food labels. Opt for products with lower sugar content or natural sweeteners like fruits.
Limit Processed Foods and Sugary Drinks: Processed foods and sugary drinks are major sources of added sugars and fructose. Limit your intake and focus on whole, unprocessed foods.
Whole Fruits in Moderation: Fruits offer essential nutrients and the benefits of fiber. Enjoy them in moderation as part of a balanced diet.
Maintain a Healthy Weight: Losing weight can improve insulin sensitivity and potentially reduce fatty liver disease.
Exercise Regularly: Exercise helps the body utilise glucose more effectively, reducing the burden on the liver.
Consult a Healthcare Professional: Discuss your concerns about fructose intake and fatty liver disease with your doctor. They can provide personalised advice and monitor your liver health.
Moderation is Key
By understanding the metabolic differences between fructose and glucose, we can make informed dietary choices. While fruits naturally contain fructose, they also offer essential vitamins and fiber. The key is moderation and limiting added sugars, particularly high fructose corn syrup, to prevent the negative consequences of excessive fructose intake and promote a healthy liver.
In conclusion, fructose may be more than just an innocent sugar; it poses significant metabolic challenges, especially to the liver, leading to a higher risk of metabolic dysfunction and obesity. Unlike glucose, fructose is metabolised in a way that bypasses many regulatory steps, overwhelming the liver and promoting fat storage rather than energy production. Understanding these unique metabolic impacts highlights why reducing excessive fructose intake is key to supporting a healthier metabolism and overall well-being. Prioritising balanced, nutrient-rich foods can help mitigate these metabolic disadvantages.



Comments