Saturated Fat, Cholesterol, and Heart Disease: Rethinking the Narrative
- S A

- Aug 6, 2025
- 12 min read
HISTORY Saturated fat has long been considered a cause of heart attacks primarily due to its association with raising LDL cholesterol levels, which are thought to contribute to atherosclerosis — the build-up of plaques in the arteries that can lead to heart attacks and strokes. This view stems from decades of research and public health policy, but it's also a topic of ongoing debate and reevaluation in the scientific community.
This long-standing belief about saturated fat and heart disease has shaped dietary guidelines for generations, leading to widespread fear of foods like butter, cheese, and red meat. However, as our understanding of lipid metabolism, inflammation, and cardiovascular risk has evolved, so too has the need to re-examine this narrative. Are saturated fats inherently harmful, or does their impact depend on the broader dietary and metabolic context in which they’re consumed? To answer that, we need to go beyond surface-level associations and explore the underlying biochemistry — starting with how different types of fat and carbohydrate affect triglyceride transport, LDL particle formation, and ultimately, cardiovascular health.
Saying "saturated fat raises LDL" without mechanistic insight is overly simplistic and sometimes misleading. Let’s dig into the biochemistry of how saturated fats influence LDL cholesterol, and clarify what’s known, what’s hypothesised, and what’s misunderstood.
What Actually Happens to Saturated Fat in the Body?
When you eat saturated fat (e.g., butter, coconut oil, animal fats), it undergoes the following steps:
1. Digestion & Absorption:
In the small intestine, saturated fats are broken down by pancreatic lipase into free fatty acids and monoglycerides.
These are absorbed by enterocytes (intestinal cells) and re-esterified into triglycerides, then packaged into chylomicrons (a type of lipoprotein).
Chylomicrons enter the lymphatic system, then the bloodstream, where they deliver triglycerides to muscle and fat tissue.
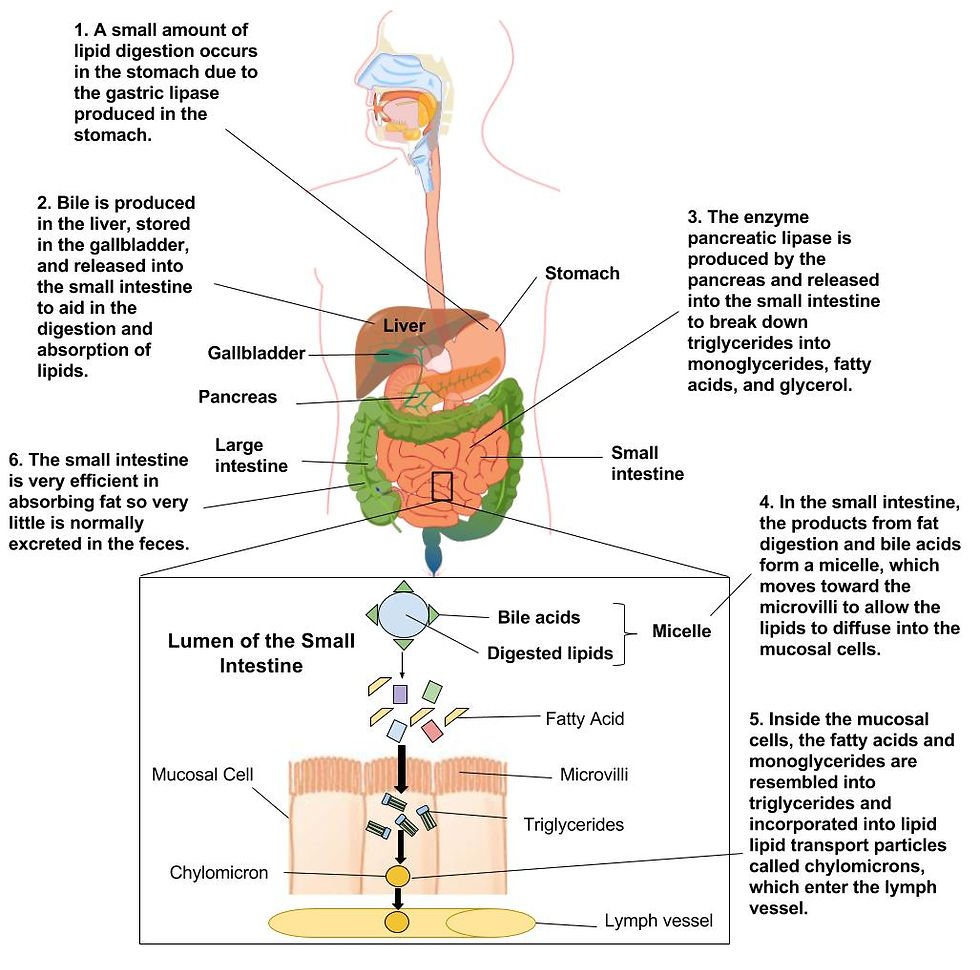
Image Credit: BCCampus
2. Distribution & Offloading:
As chylomicrons circulate through the bloodstream, they encounter lipoprotein lipase (LPL) — an enzyme anchored on the capillary walls of muscle and adipose tissue.
Insulin plays a key role here, activating LPL particularly in fat tissue, allowing triglycerides to be offloaded and taken up by cells for storage or energy use.
Muscle tissue tends to burn the fat for energy (especially in insulin-sensitive, low-carb states), while adipose tissue stores it when insulin is high (e.g., after a high-carb meal).
The more efficiently this offloading happens, the smaller the chylomicron remnant that returns to the liver — meaning less leftover triglyceride and cholesterol for the liver to process.
Remnants now circulate systemically, passing through arteries, including coronary and cerebral arteries before returning to the liver.
Unlike LDL, which may need to be oxidised to trigger atherogenesis, remnant cholesterol is atherogenic “as-is.” Here's why:
Smaller size than chylomicrons allows remnants to penetrate the endothelial lining.
They are cholesterol-rich, and once trapped, they can:
Promote foam cell formation.
Trigger inflammation (via macrophages and TLR4).
Contribute to plaque growth and instability.
Key point: The longer remnants circulate (e.g. in insulin resistance, metabolic syndrome), the greater the opportunity for arterial damage.
Note: While adipose tissue and skeletal muscle are the primary sites for triglyceride (TG) offloading from chylomicrons via lipoprotein lipase (LPL), other tissues also take up free fatty acids (FFAs) and triglyceride-derived lipids, though to a lesser extent and usually under specific physiological conditions.
Cardiac Muscle (Heart)
Very active in oxidising FFAs, especially during fasting, exercise, or low-carb states.
The heart has high LPL activity and takes up FFAs from circulating chylomicrons and VLDL.
Preferentially uses fat as fuel unless under high glucose/insulin conditions.
Brown Adipose Tissue (BAT)
Specialised in thermogenesis and burns FFAs for heat production.
Has high LPL activity and takes up FFAs, especially in cold exposure or in infants (more active BAT).
Recent interest in BAT’s role in metabolic health is growing.
Lactating Mammary Glands
In breastfeeding women, mammary glands use LPL to take up TGs from chylomicrons to synthesise milk fat.
This is one of the only non-storage roles of chylomicron TGs outside energy metabolism.
3. Liver Processing:
Chylomicron remnants return to the liver.
The liver uses the remaining fat (along with excess dietary carbs and protein) to synthesise VLDL (very low-density lipoproteins).
These VLDLs are secreted into the bloodstream and progressively lose triglycerides via lipoprotein lipase, becoming IDL and eventually LDL particles.
Key Point: LDL is not made directly from saturated fat, but through a cascade involving VLDL metabolism. Saturated fat may influence how much VLDL the liver makes, and how LDL is processed or cleared. Most dietary fat is delivered to muscle or fat cells, but depending on context — fasting, insulin levels, inflammation, or cold exposure — other tissues play critical and sometimes overlooked roles in fat metabolism.
Why the Liver Sends Out VLDL After Chylomicrons
At first glance, it might seem redundant: if chylomicrons have already delivered dietary fat from the gut and returned to the liver as remnants, why does the liver turn around and send out more fat in the form of VLDL (very low-density lipoproteins)?
The answer lies in the distinct roles, metabolic context, and flexible logistics of lipid transport. Chylomicrons are designed for post-meal delivery of dietary fat. They’re massive, triglyceride-rich particles that offload fat primarily to adipose and muscle tissues with the help of lipoprotein lipase (LPL). Whatever remains — mostly cholesterol, phospholipids, and some triglycerides — is returned to the liver as a chylomicron remnant.
But the liver doesn’t just “discard” these remnants. Instead, it repackages leftover dietary fat, along with:
Free fatty acids taken up from the bloodstream,
Triglycerides newly synthesised from excess carbohydrates (via de novo lipogenesis),
And internal lipid stores,
…into VLDLs. These smaller, denser particles serve a different purpose: they provide a steady supply of energy to tissues between meals, during fasting, or in low-carb states. This makes VLDLs a key component of the liver’s long-term lipid logistics — far more than a simple rerun of chylomicron delivery.
Importantly, VLDL production is highly influenced by your metabolic state. In insulin-resistant or overfed conditions, VLDLs are often overloaded with triglycerides, leading to small, dense LDL particles downstream — a known cardiovascular risk factor. In contrast, under low-insulin, fat-adapted conditions, VLDLs are leaner, and the resulting LDL particles tend to be large and buoyant, with a much lower atherogenic profile.
Bottom line: The liver doesn’t resend the same fat for no reason. VLDL output reflects the body’s ongoing need to allocate energy, especially when carbohydrate availability, insulin levels, and energy balance shift. It’s not redundancy — it’s strategic, dynamic redistribution.
How Might Saturated Fat Increase LDL Cholesterol?
Here are three main mechanisms proposed in the literature:
1. Downregulation of LDL Receptors (LDL-R) in the Liver
Saturated fats may reduce LDL receptor activity, meaning less LDL is cleared from the bloodstream.
This effect has been shown in some cell and animal studies and is partly mediated by SREBP-2, a transcription factor regulating LDL-R and cholesterol synthesis.
The liver senses it has "enough" cholesterol, so it reduces receptor expression — leading to higher circulating LDL.
But caveat: This effect may depend on overall metabolic health. In insulin-resistant or inflamed states, LDL-R function may already be impaired — regardless of saturated fat intake.
Which Saturated Fats Are Most Implicated?
Saturated Fat | Carbon Chain | Source | Effect on LDL/LDL Receptor |
Palmitic acid (C16:0) | 16 | Meat, dairy fat, palm oil | Most associated with reduced LDL receptor activity and higher LDL-C. |
Myristic acid (C14:0) | 14 | Butter, coconut oil | Potent LDL-C raiser — may reduce LDL receptor activity more than palmitic. |
Lauric acid (C12:0) | 12 | Coconut oil | Raises LDL, but also raises HDL significantly; effect on LDL receptor less clear. |
Stearic acid (C18:0) | 18 | Cocoa butter, beef fat | Neutral effect on LDL receptor activity; doesn’t raise LDL-C much — often considered "cardio-neutral." |
Key point: Palmitic and myristic acids are the most likely to reduce LDL receptor activity. Stearic acid is generally neutral.
2. Influence on Hepatic VLDL Production
Some saturated fatty acids, particularly palmitic acid, may stimulate the liver to produce more VLDL.
More VLDL secretion means more eventual LDL in circulation.
This may happen via upregulation of de novo lipogenesis, especially when combined with excess carbs.
3. Particle Size and Number
Saturated fat tends to increase larger, buoyant LDL particles, while low-fat, high-carb diets often increase small, dense LDL (which are more atherogenic).
Many recent studies argue LDL particle number (LDL-P) and apoB are more predictive of cardiovascular risk than LDL-C (the cholesterol content).
LDL Increase ≠ Automatically Harmful
Even when saturated fat raises LDL, it's not always bad:
It may raise HDL cholesterol as well, improving the total cholesterol / HDL ratio.
The LDL may shift to larger, less atherogenic forms.
If the individual has low inflammation, good insulin sensitivity, and low triglycerides, the atherosclerotic risk may be low despite a rise in LDL.
Additional Factors That Modulate the Response
Saturated fat’s effect on LDL is contextual:
Genetics: Some people are “hyper-responders” to dietary fat.
Insulin resistance: In metabolic syndrome, the liver is already pumping out VLDL.
Gut microbiome: May play a role in lipid metabolism and inflammation.
Overall diet: A diet high in saturated fat plus refined carbs (e.g., junk food) is far more damaging than saturated fat in a whole-food, low-carb context (e.g., ketogenic diet).
Summary
Saturated fats do not directly become LDL, but may influence how much LDL circulates via:
Downregulating liver LDL receptors, reducing clearance
Increasing hepatic VLDL secretion, leading to more LDL
Changing LDL particle size and composition
But the response is highly individual and context-dependent. In metabolically healthy individuals eating whole foods, saturated fat may have neutral or even favourable effects on lipid profiles.
So the simple claim “saturated fat raises LDL, therefore causes heart attacks” is outdated. A more accurate view must consider biochemistry, particle quality, metabolic health, and dietary context.
Understanding what happens to Chylomicrons
The lipoprotein particles that transport dietary triglycerides (TGs) from the intestine — is key to grasping how different diets influence lipid metabolism. Specifically, the proportion of TGs that chylomicrons offload to muscle and fat tissue versus how much returns to the liver as remnants can vary dramatically depending on dietary context. Whether the diet is rich in saturated fats combined with high carbohydrates (especially ultra-processed ones) or follows a low-carbohydrate, higher-fat approach can radically alter these metabolic outcomes. To make sense of this, let’s break it down into three parts.
1. What Determines How Much Triglyceride (TG) from Chylomicrons Is Offloaded?
When chylomicrons enter the bloodstream, their fate is influenced by:
a. Lipoprotein Lipase (LPL) Activity
LPL is the key enzyme that hydrolyses TG in chylomicrons so free fatty acids (FFAs) can be taken up by tissues.
It’s anchored on capillary walls in muscle, heart, adipose tissue.
LPL activity is regulated by:
Insulin: Boosts LPL in adipose tissue, suppresses it in muscle.
Fasting: Boosts LPL in muscle, so FFAs are used for energy.
Fed state (esp. high-carb): LPL is up in fat, storing fat.
Exercise: Increases muscle LPL → more fat burned for fuel.
Inflammation or insulin resistance: Impairs LPL, so TGs hang around longer in the blood.
b. Tissue Demand for Energy or Storage
Active muscles will grab FFAs for energy.
Adipose tissue stores TGs during the fed state.
Liver takes up chylomicron remnants with leftover TG and cholesterol.
So, how much TG is offloaded vs. sent to the liver depends on LPL function, insulin signalling, and energy needs.
2. What Happens in a High-Carb + Saturated Fat (esp. Ultra-Processed) Context?
This is metabolically the worst case. Here’s how it plays out:
a. Postprandial State Flooded with Insulin
High-glycaemic carbs cause insulin spike.
Insulin drives LPL to adipose tissue → promotes fat storage, not oxidation.
Saturated fat from chylomicrons is offloaded preferentially to fat stores.
b. Liver Becomes a Dumping Ground
Excess chylomicron remnants, plus glucose-driven de novo lipogenesis (DNL), create a double TG load in the liver.
Liver packages this as VLDL, adding to circulating TGs and eventually LDL.
c. Insulin Resistance Worsens the Cycle
Over time, insulin resistance:
Decreases LPL efficiency.
Causes more TG to remain in chylomicrons.
Impairs hepatic clearance of remnants.
Increases VLDL overproduction → small dense LDL + high apoB.
Net result: More chylomicron remnants return to liver, more VLDL is produced, higher postprandial lipemia, and more atherogenic particles.
3. What Happens in a Low-Carb + Saturated Fat Context?
Here, the scenario is almost reversed:
a. Low Insulin = Shift to Fat Oxidation
Low insulin means:
Muscle LPL increases.
Adipose LPL decreases → less fat storage.
Muscles and heart grab FFAs for fuel.
b. Less Chylomicron Remnant Burden on Liver
More TGs are offloaded and used by tissues → fewer leftovers for the liver.
Less substrate for VLDL production = lower circulating TG and less LDL formation.
c. Ketogenic Adaptation
In keto or low-carb states, fat becomes the primary fuel.
Liver may use incoming chylomicron-derived FFAs to make ketones, not VLDL.
Net result: Efficient TG offloading, fewer chylomicron remnants, lower TG/HDL ratio, and less hepatic lipogenesis.
4. Summary: High Carb vs Low Carb Impact on Chylomicron Remnants
Parameter | High-Carb + Sat Fat (esp. ultra-processed) | Low-Carb + Sat Fat |
Insulin | High | Low |
LPL Activity | ↑ in adipose, ↓ in muscle | ↑ in muscle, ↓ in fat |
TG Offloading | Mostly to fat stores | Mostly to energy-hungry tissue |
Chylomicron Remnants | More return to liver | Fewer remnants |
Liver burden | High (remnant + DNL) | Low |
VLDL Output | Increased | Reduced |
Atherogenic LDL Risk | Higher (esp. small dense LDL) | Lower (larger LDL) |
Another important perspective to consider is the impact of a high-carbohydrate, low-saturated fat diet — particularly when distinguishing between ultra-processed carbohydrates and those from whole-food sources. This distinction matters because not all carbohydrates are created equal, and simply reducing saturated fat intake doesn’t necessarily translate into lower cardiovascular risk, especially when ultra-processed foods dominate the diet. To fully understand this dynamic, we need to explore it across several dimensions: metabolic effects, cholesterol and lipoprotein profiles, energy intake and expenditure, and overall implications for heart health.
Metabolic and Energy Impact
Ultra-Processed High-Carb + Low Saturated Fat
Hyperpalatable and calorie-dense: Easy to overeat due to low fibre, high reward value, fast digestion.
Rapid glucose spikes → large insulin surges → promote fat storage and inhibit fat oxidation.
Frequent hunger: Low satiety leads to increased energy intake.
Lower energy expenditure: Processed diets reduce thermic effect of food (TEF) and metabolic rate.
Net result: Positive energy balance, weight gain, higher adiposity, metabolic inflexibility.
Whole-Food High-Carb + Low Saturated Fat
Slow-digesting, fibre-rich: Promote satiety, stable glucose and insulin.
Less insulin spike, better nutrient partitioning.
Moderate energy intake: Harder to overeat.
Higher TEF: More energy spent digesting real food.
Net result: Neutral to mildly positive energy balance; metabolically stable in active individuals.
Lipids and LDL Cholesterol
Ultra-Processed High-Carb + Low Saturated Fat
Increases de novo lipogenesis (DNL) in liver → TG production → ↑ VLDL → eventually small dense LDL.
Lowers HDL and increases TG/HDL ratio (a marker of insulin resistance).
Increases inflammatory markers (e.g., CRP).
Higher apoB and particle number → more atherogenic lipoproteins.
Whole-Food High-Carb + Low Saturated Fat
Minimal DNL (unless overfed).
May lower LDL-C modestly, especially in low-fat diets.
Improves TG and HDL if calorie-controlled and low glycaemic.
Less oxidative stress and inflammation.
ApoB remains stable or may improve.
Net result: Ultra-processed carbs damage lipid metabolism; whole carbs may be neutral or even protective in healthy individuals.
Energy Intake and Expenditure
Diet Type | Energy Intake | Satiety | Thermic Effect | Fat Oxidation | Insulin | Hunger |
Ultra-processed high-carb | High | Low | Low | Inhibited | High | Frequent |
Whole-food high-carb | Moderate | High | Moderate | Mildly inhibited | Moderate | Stable |
Cardiovascular Risk
Ultra-Processed High-Carb + Low Saturated Fat
Despite low saturated fat, it’s associated with:
Obesity
Insulin resistance
Metabolic syndrome
Elevated TG, low HDL, small dense LDL
High apoB, high particle count
Chronic inflammation
Strongly linked to CVD, type 2 diabetes, and NAFLD.
Conclusion: Low saturated fat doesn’t protect the heart if replaced with ultra-processed carbs.
Whole-Food High-Carb + Low Saturated Fat
Can be heart-protective when:
Paired with high fibre, polyphenols, and micronutrients.
Energy intake is appropriate.
Physical activity is adequate.
Lower LDL-C, improved endothelial function, and lower CRP.
Examples: Traditional Okinawan or high-fibre Mediterranean diets.
Conclusion: Whole-food high-carb diets can be heart-healthy when calorie-controlled and part of an active lifestyle.
Summary Table
Diet | Insulin Response | LDL Profile | TG/HDL Ratio | Energy Intake | CVD Risk |
High-carb, ultra-processed | High (spikes) | ↑ Small dense LDL | High | High | High |
High-carb, whole foods | Moderate | ↓ or neutral | Low | Moderate | Low-to-moderate |
Low-carb, high saturated fat | Low | ↑ Large LDL (not atherogenic) | Low | Moderate | Contextual |
Key Differences in Chylomicron Offloading Across These Diets:
Diet Type | Insulin Effect | LPL Activity Favouring | TG Offloading Efficiency | Likely LDL Outcome |
High-carb, ultra-processed | High, erratic | Adipose > muscle | Poor (↑ remnant TGs) | Small, dense LDL |
High-carb, whole-food | Moderate, stable | Balanced | Improved vs processed | Mixed, often neutral |
Low-carb, high sat fat | Low | Muscle/heart > adipose | High (↑ oxidation) | Large, buoyant LDL |
Conclusion: A New Look at an Old Villain
For decades, saturated fat has been cast as the dietary villain behind heart disease — largely because of its association with elevated LDL cholesterol. But as we've unpacked in this deep dive, the story is far more nuanced.
Saturated fats don’t act in isolation. Their metabolic fate — from digestion in the gut to repackaging in the liver — is profoundly shaped by the company they keep: namely, carbohydrates (especially refined ones), insulin levels, activity patterns, and inflammation. Whether saturated fat ends up being stored, oxidised for energy, or contributing to atherogenic lipoprotein profiles depends less on its presence and more on the metabolic context in which it’s consumed.
We saw how low-carb, fat-adapted states promote efficient chylomicron offloading, favour muscle and heart tissue uptake, and typically result in large, buoyant LDL particles — far less harmful than their small, dense counterparts. In contrast, diets high in ultra-processed carbohydrates — even when low in saturated fat — tend to impair fat partitioning, elevate triglycerides, promote small dense LDL, and drive metabolic dysfunction over time.
It's clear that the combination and quality of macronutrients — not saturated fat alone — determine whether lipids become fuel or feed the fire of cardiovascular disease. The time has come to move beyond outdated dietary dogma and embrace a more nuanced, systems-based understanding of how fat, insulin, and inflammation interact in the body. The real question isn't whether saturated fat raises LDL — it's how and where those fats are being used in the metabolic ecosystem.
In the next blog, we'll go even deeper into the heart of the debate: What exactly is LDL cholesterol? Is all LDL created equal? And how should we rethink our approach to saturated fat, cholesterol, and heart disease risk in the modern era?
*Disclaimer:
The information provided in this blog is for educational and informational purposes only and should not be construed as medical advice. While every effort is made to ensure accuracy, the content is not intended to replace professional medical consultation, diagnosis, or treatment. Always seek the guidance of a qualified healthcare provider with any questions regarding your health, medical conditions, or treatment options.
The author is not responsible for any health consequences that may result from following the information provided. Any lifestyle, dietary, or medical decisions should be made in consultation with a licensed medical professional.
If you have a medical emergency, please contact a healthcare provider or call emergency services immediately.




Comments